Arrival and first impressions
The thought of going to Florence, Italy for a one-week practical exposure on Clinical Risk management and Patient Safety left me very anxious. It will be my first time travelling to Italy, and secondly, I was eager to have an Italian experience in the course of my fellowship training. Italians are known for their hard work, prowess, determination and novelty. Italy is almost synonymous to ‘authenticity’, and I knew that their pursuit for quality in health care (especially patient safety) will not be any different.
As I arrived Italy on the evening of Sunday, 15th June 2019, I beheld the beauty and authenticity of her cities from Milan (where I landed) to Florence (where I will be residing). The magnificence of its Cathedral, solidness of the architecture, through the uniqueness of its canals and the stone-paved streets were a confirmation of the originality of the Italian people, their institutions and the culture therein. My expectations for the intellectual resources I was going to take with me from Italy to Africa grew in depth and breadth with every minute that passed.

Encounter with the Centre for Clinical Risk management and Safety (GRC)
Thanks to the special logistic skills of the ISQua secretariat, I resided at a Mini-Residence which was 10 minutes away from the GRC (Centro Gestione Rischio Clinico e Sicurezza del Paziente). The GRC is a clinical governance structure instituted in 2003 by the Tuscan regional council. The embryo of this centre was the Ergonomics and Human Factors Research Centre in Healthcare which was founded in 2000 by the joint efforts of the Florence Healthcare Trust, the University of Florence and Siena. GRC promotes a safety culture within health facilities in the region through active and cross-disciplinary learning from adverse events and medical errors. This centre has a formidable team from multi-disciplinary backgrounds comprising of public health experts, clinical risk managers, experts in law, psychology, communication, human factors and organisational studies. It is the mother regional centre for patient safety that has inspired the creation of similar centres in Italy. GRC Toscana is headed by Dr Riccardo Tartaglia, who is the pioneer director.

Italian network for Safety in Healthcare
My visit coincided with an important event in the life of patient safety improvement efforts in Italy – The Italian Network for Safety Conference. I was indeed very privileged to be part of such a memorable event which was organised to reflect on the journey of the patient safety movement and the way forward. Most importantly, it was a unique moment to appreciate the great works of its founder and pioneer president, Dr Riccardo Tartaglia (who was retiring).
This network was formed in 2004. It is a forum that brings together experts in patient safety across the country to enhance the culture of safety in healthcare. The experts took turns as they presented the groundbreaking research they have conducted on safety in healthcare. It was amazing how all the speakers took their hats off to the outgoing Director.

The height of this conference for me was getting to know how instrumental this body of experts has been the force behind the enactment of the Italian law on patient safety in 2017, recognizing patient safety as a fundamental human right. The importance of human factors, care processes, training and a just culture was a common thread that ran through most of the presentations. I was opportune to make contacts with and join very rich professional networks on patient safety.
Field visits to observe patient safety practices
As part of my programme, I visited two health institutions. The first was the Meyer Paediatric Hospital.

It was a great pleasure to have met with Professor Antonino Morabito who introduced me to the safety culture and practices in the theatre and surgical care at the hospital. Amongst many practices, the use of a surgical checklist was particular. The hospital has adapted the WHO surgical checklist into an easy to use assessment tool.
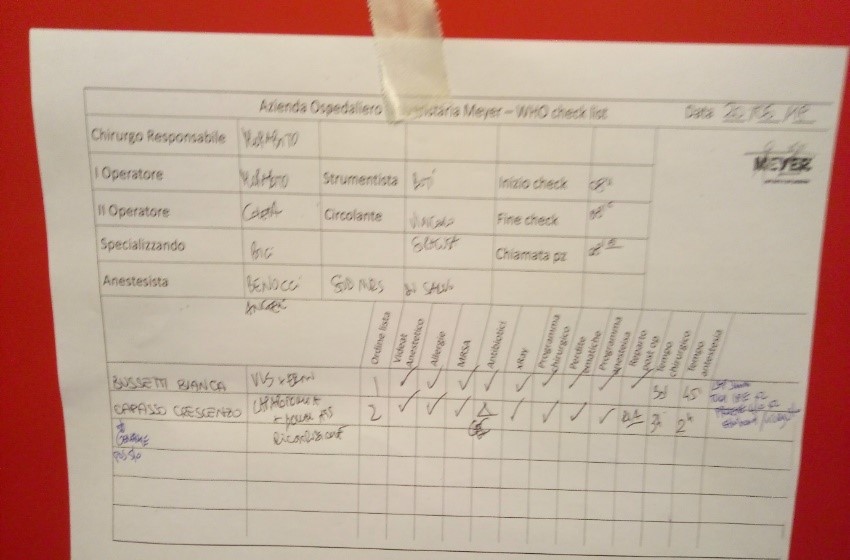
This tool is checked by the entire surgical team and their colleagues who have patients to undergo surgical operations in the theatre in the morning of the day scheduled for the procedure.

The hospital has trained Clinical Risk Managers who support the patient safety facilitators in all the units of the hospital. I was privileged to work with Angella and Klaus who literally took me by the hand through the various units of the hospital exhibiting the patient safety practices. These practices included; hand hygiene, pain management, falls (adults & paediatric), Central Venous catheterization, patient unique identification, checklists, antibiotic use, blood transfusion, bed ulcer prevention/management, reporting and learning system, handing-over procedure, effective communication and clinical audits.
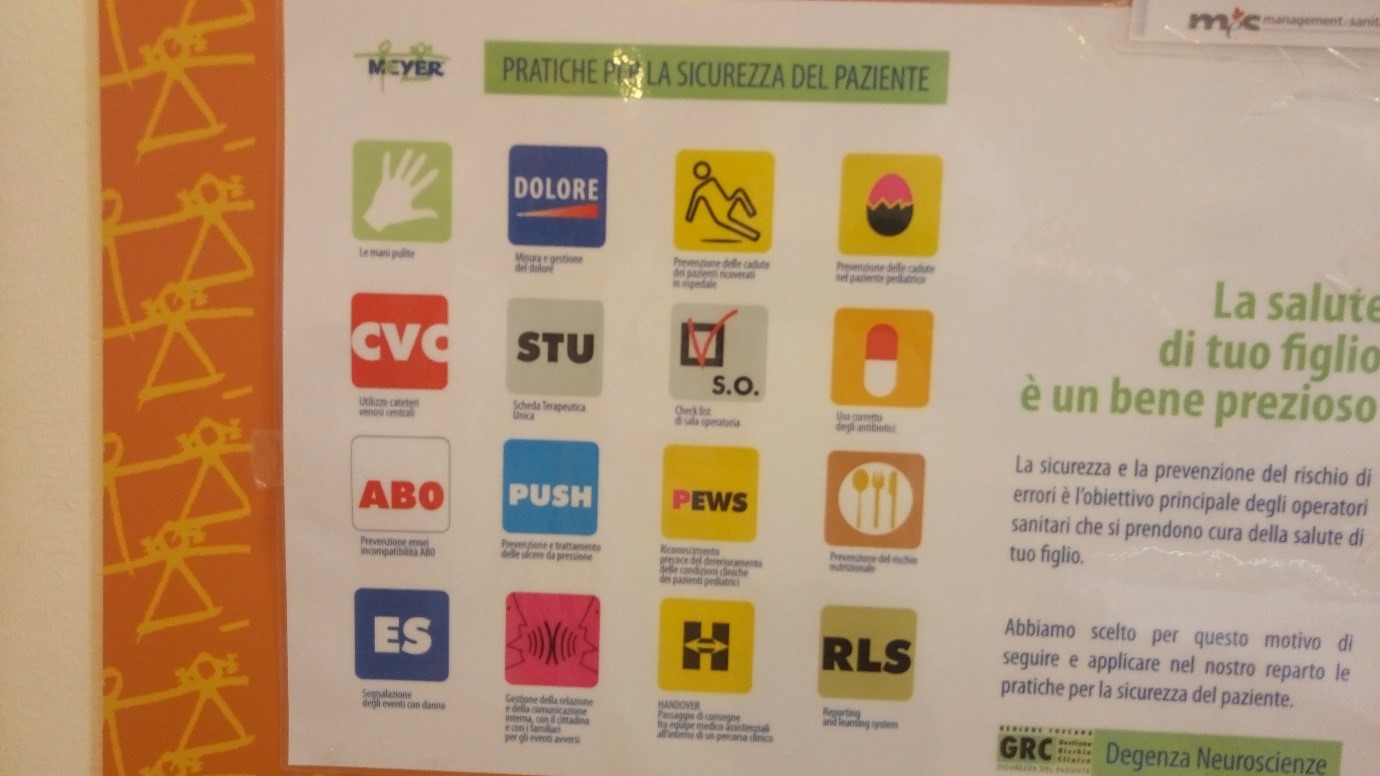
For the sake of brevity, I will present just a tip of the iceberg – two of the sixteen patient safety practices. These guidelines and best practices have been tested by the regional centre for safety before validation by the National Institute for Safety.
Hand hygiene practices were very prominent in all units of the hospital. To reinforce the WHO hand hygiene campaign, all entrances to the hospital, alleys, nursing stations and wards were dotted with hand washing stations (washing sinks with liquid soap or hand sanitiser dispensers).

Another very striking patient safety practices were concerning medication safety. These included the ‘Look-Alike-Sound-Alike’ (LASA) approach which was used in the arrangement of medications in drug shelves. The ‘LASA’ drugs were identified by a yellow label, while high-risk medications were identified by a ‘High-level attention’ red label. Medications like Morphine, which were liable to abuse were locked up in a closet and the keys of the closet were handed to a particular nurse in each shift.

Visit to the Santa Maria Hospital
The Santa Maria Hospital was the second facility selected for my field visit. I participated in a clinical audit conducted to clarify the best management plan for a patient who was erroneously hospitalised in the internal medicine ward of the hospital. The audit was attended by all the unit heads/specialists, nurses, residents and General Practitioners involved in the care of the patient. In attendance was also a Clinical Risk Manager. The audit was done using the Failure Mode and Effect Analysis (FMEA) approach. The manner in which this audit was conducted to arrive at three key resolutions was very fascinating and eye-opening.
Collaborating role of the GRC
One of the functions of the GRC is to serve as a collaborating centre for WHO in improving patient safety around the world. To this end, the objectives of the centre include:
- To develop global online knowledge sharing platforms. These will serve to collect best practices on patient safety, especially those that are context-specific (Grey experiences) and not necessarily evidence-based practices.
- Collect and share patient safety incidents with the aim of learning through a structured analysis of events to develop knowledge,
- To support WHO to promote and implement patient safety. For example, medical safety, surgical safety, hand hygiene etc.
The centre applies the six-step approach for Twinning Partnership for improvement to establish collaborations. It is currently collaborating with two hospitals in Kenya and seventeen hospitals in Palestine to implement the WHO Safe Child Birth Checklist to improve maternal and child health. The approach adopted for these collaborations is basically in 3 phases: the checklist is piloted in the facility; it is adapted with feedback from the piloted facilities, and then the adapted checklist is implemented, and the impact evaluated.
What did I take home?
From this rich encounter, which I have summarised in this write up, I have accepted that quality improvement and patient safety, in particular, can be achieved when there is a professional and political commitment. With all the tools and knowledge which I have acquired within one week, I intend to start to ignite a patient safety movement in my setting. With the support of the GRC via a collaboration with two regional hospitals in my region and a Civil Society Organisation (FALCOH) which I co-founded, I believe that patient safety can be achieved in my setting in the near future.
I sincerely thank ISQua for offering me this great learning and networking opportunity.
